LITTLE ROCK, Ark. — The national emergency declared in March 2020 allowed the federal government to take steps to respond to the coronavirus supporting the country's economic, health, and welfare systems.
It is now three years later and that help is coming to an end.
So, here's how it might impact you.
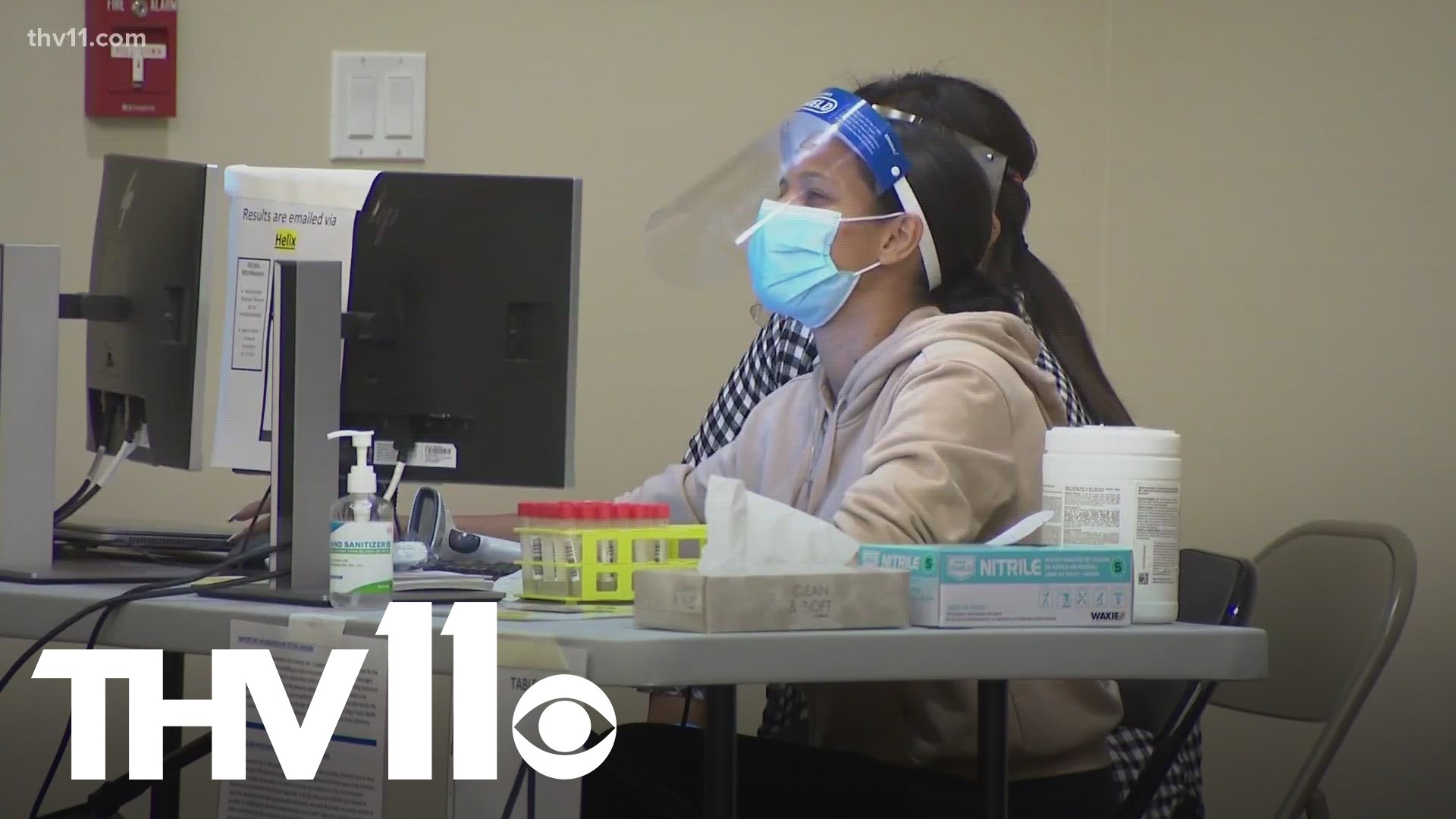
One of the biggest changes is the cost of COVID-19 tests.
According to the U.S. Department of Labor, your insurance plan may no longer be required to cover the costs of over-the-counter tests.
You might be responsible for paying all or part of the cost, but it depends on your insurance provider
Second, is COVID-19 vaccinations. Your health insurance could now require you to pay if you get a vaccine from a place not in your health plan's network.
Third is telehealth which is something that became popular in the past few years. A lot of health insurance plans expanded to include it, but that may no longer be the case, again depending on your plan.
Medicaid coverage could also change. If you or your family members are covered by Medicaid now is the time to check if your coverage will continue.
“The renewal packets have been going out and we've been preparing for this for more than a year,” said Gavin Lesnick with DHS. “You know, we didn't know exactly when the public health emergency would end. But we knew a year ago that was on the horizon.”
Lesnick also explained that those who qualify will keep their coverage, and those who don't will be transitioned to a different plan
“During the public health emergency beneficiaries on Medicaid, for the most part, couldn't lose coverage. Even if their circumstances changed, and they were no longer qualified for the program, they were not disenrolled,” said Lesnick. “But now with the ending of the public health emergency that's changing.”
DHS has been reaching out to Arkansans since February and reminding people to keep a close eye on the mail.
"It's something we've been preparing for, and reaching out to beneficiaries, making sure that they're aware that a change is coming, asking them to update their address and their contact information so we can reach them," said Lesnick.
If you're unsure where you stand when it comes to Medicaid eligibility and renewal, please click here.